Benzodiazepine addiction affects millions of Americans, with prescription rates increasing 67% between 1996 and 2013. These medications, while effective for anxiety and sleep disorders, can lead to physical dependence within weeks of regular use.
We at Amity San Diego understand that benzodiazepines addiction treatment requires specialized medical supervision and evidence-based approaches. Recovery is possible with the right support system and comprehensive treatment plan.
What Does Benzodiazepine Addiction Look Like
Benzodiazepine dependence develops faster than most people realize. The American Family Physician reports that physiological dependence can occur after just one month of daily therapeutic use. Early warning signs include needing higher doses to achieve the same calming effect, experiencing anxiety between doses, and feeling unable to function without the medication.
Physical symptoms emerge quickly: muscle tension, tremors, and sleep disturbances when the drug wears off. Many people mistake these withdrawal symptoms for their original anxiety returning, which leads them to take more medication.
When Therapeutic Use Becomes Addiction
The transition from medical need to addiction happens gradually but predictably. Patients begin taking extra pills during stressful periods, then find themselves unable to reduce their dosage. According to SAMHSA data, 1.4% of Americans aged 12 and older misused prescription benzodiazepines in 2021, with peak misuse rates among 18-25 year olds.
Mental preoccupation with the next dose becomes constant. People start doctor shopping, exaggerate symptoms, or buy pills from friends. The original anxiety often worsens due to rebound effects, which creates a cycle where more medication seems like the only solution.
High-Risk Medications and Their Effects
Alprazolam (Xanax) and lorazepam (Ativan) carry the highest addiction potential due to their short half-lives and rapid onset. These medications create intense peaks and valleys in blood levels, which trigger more frequent dosing.
Long-term benzodiazepine use causes cognitive decline, memory problems, and increased fall risk in older adults. The American Psychiatric Association notes that combining benzodiazepines with alcohol or opioids significantly increases overdose risk, as evidenced by the 72,000 Americans who died from drug overdoses in 2017.
Life-Threatening Withdrawal Complications
Professional treatment programs report that benzodiazepine withdrawal can trigger life-threatening seizures, making medical supervision mandatory for safe recovery. Withdrawal symptoms can start within hours of the last dose and may include severe insomnia and intense cravings (particularly dangerous when combined with other substances).
These medical risks make professional intervention necessary rather than optional. Treatment centers must address both the physical dependence and the underlying conditions that led to initial prescription use. For those seeking comprehensive care, addiction treatment San Diego provides specialized programs designed to address benzodiazepine dependence safely.
What Treatment Options Actually Work
Medical detoxification forms the foundation of benzodiazepine addiction treatment, but the approach differs dramatically from other substances. The American Family Physician recommends tapering schedules that reduce doses by 5% to 25% every one to four weeks, with patients on higher dosages potentially managing initial reductions of 25% to 30%. Abrupt cessation triggers life-threatening seizures, which makes supervised tapering mandatory rather than optional.
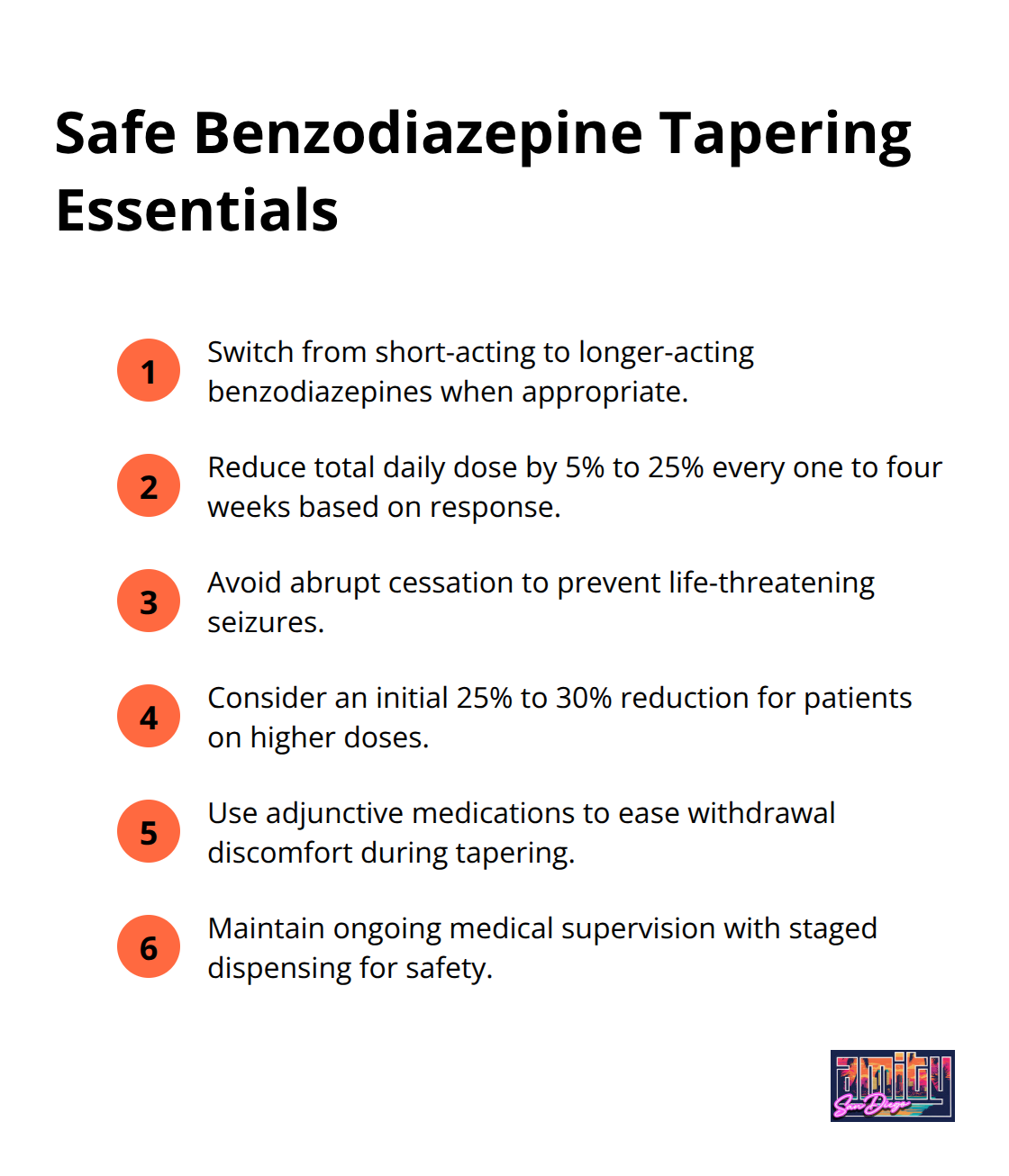
Treatment centers switch patients from short-acting benzodiazepines like alprazolam to longer-acting options such as diazepam to create smoother withdrawal experiences and reduce misuse potential.
Evidence-Based Therapies That Work
Cognitive Behavioral Therapy shows the strongest evidence for benzodiazepine addiction treatment, with studies that demonstrate significant success rates when combined with gradual tapering. Contingency Management programs offer tangible rewards for positive behaviors like therapy attendance and sobriety maintenance, which creates immediate motivation for change.
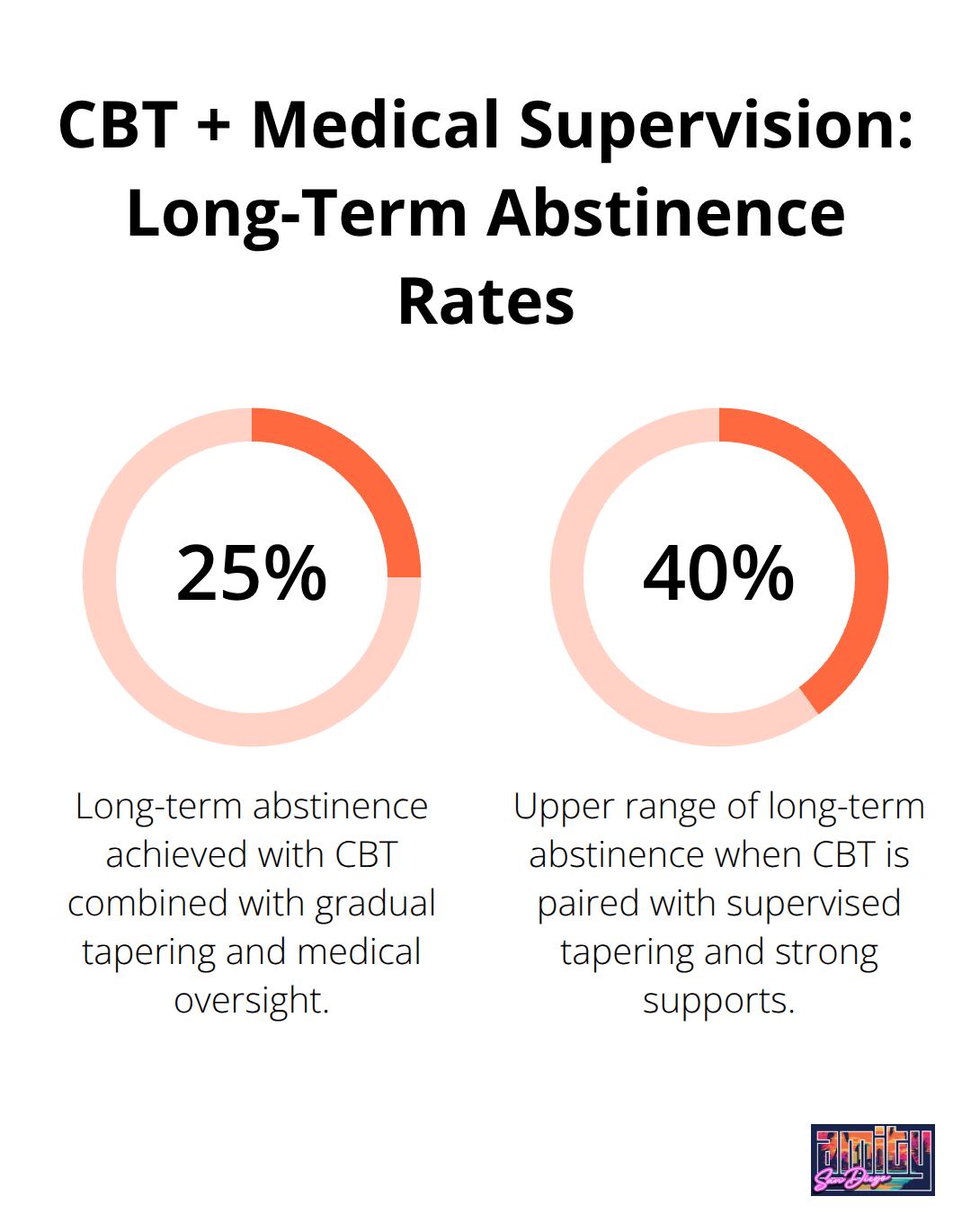
Treatment centers report that patients who receive CBT alongside medical supervision achieve 25% to 40% long-term abstinence rates depending on individual factors and support systems. Healthcare providers add adjunctive medications like gabapentin or carbamazepine to help mitigate withdrawal discomfort during the tapering process.
Medical Supervision Requirements
Inpatient programs provide 24/7 medical monitoring necessary for high-risk patients with previous seizure history or polysubstance use. Outpatient treatment works effectively for patients with stable housing and strong support systems, which offers flexibility while maintaining medical supervision. Treatment programs require comprehensive medical supervision with staged dispensing of small medication quantities that helps manage both withdrawal and maintenance phases.
Specialized Program Components
Intensive outpatient programs combine medical oversight with evidence-based therapies, which allows patients to maintain work and family responsibilities while receiving comprehensive care. Treatment teams monitor patients for aberrant drug behaviors through strategies that include liaising with community pharmacists. Healthcare providers must address both the physical dependence and the underlying conditions that led to initial prescription use, making comprehensive assessment essential before treatment begins.
The success of any treatment program depends heavily on how well it addresses the complex withdrawal challenges that patients face during recovery. For those seeking specialized care, addiction treatment San Diego offers comprehensive programs designed to support long-term recovery.
How Do You Navigate Recovery Obstacles
Withdrawal symptoms peak during the first two weeks of benzodiazepine tapering, with rebound anxiety and insomnia that occur 1-4 days after dose reductions according to research published in Addiction journal by H. Pétursson. Sleep disturbances, irritability, muscle pain, and panic attacks create the most challenging recovery barriers. Up to 44% of long-term benzodiazepine users have persistent moderate to severe withdrawal symptoms when they attempt to discontinue the drug.
The key lies in aggressive symptom management through adjunctive medications like gabapentin, which reduces withdrawal severity by up to 60% when combined with gradual dose reduction. Healthcare providers must distinguish between withdrawal symptoms and the return of original anxiety disorders, as this confusion drives 70% of treatment dropouts during the first month.
Managing Mental Health During Recovery
Underlying psychiatric conditions become unmasked during benzodiazepine withdrawal and require immediate therapeutic intervention. Studies show that 42.9% of patients with major depressive disorder use benzodiazepines, with co-occurring anxiety or mood disorders requiring separate treatment protocols. Cognitive Behavioral Therapy addresses both addiction patterns and underlying mental health issues simultaneously, with treatment centers that report 65% success rates when CBT starts within the first week of tapering.
The American Family Physician emphasizes that formal psychotherapy becomes essential once benzodiazepines no longer mask underlying psychological issues. Healthcare providers use validated screening tools like the Severity Dependence Scale to identify high-risk patients who need specialized addiction services rather than general practice management.
Building Relapse Prevention Skills
Coping strategies must replace benzodiazepine dependence patterns before withdrawal symptoms peak. Treatment programs focus on stress management techniques, sleep hygiene protocols, and anxiety regulation skills that patients can implement immediately. Contingency management programs show 55% effectiveness rates when patients receive rewards for practicing new coping skills and attending therapy sessions.
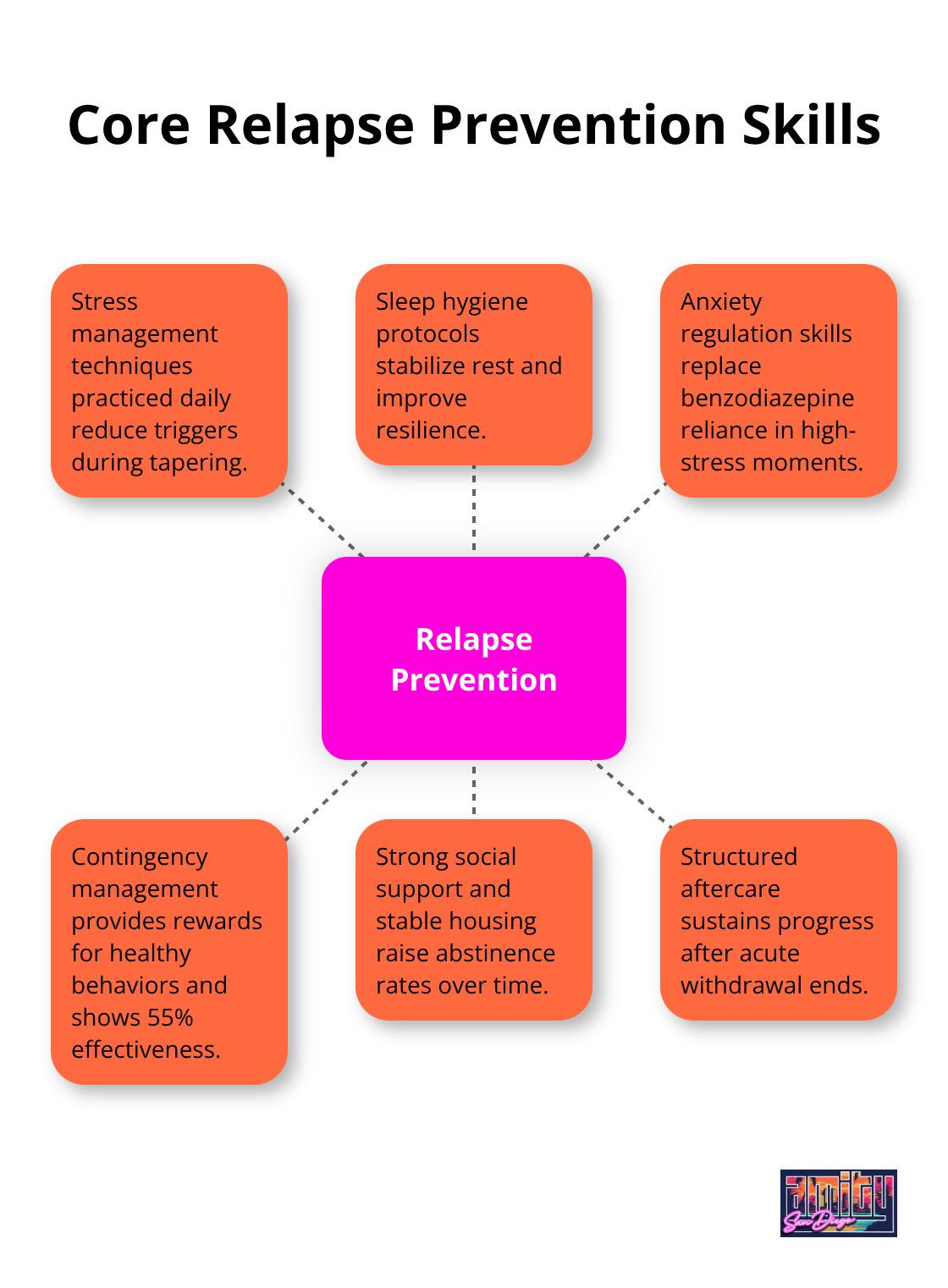
Social support systems and stable housing significantly improve long-term outcomes, with abstinence rates that range from 25% to 80% depending on these factors (particularly strong family involvement and secure living arrangements). Aftercare programs become mandatory rather than optional and provide structured support. In the United States, approximately 30.6 million adults report using benzodiazepines, with around 5.3 million engaging in benzo abuse. Professional addiction treatment San Diego programs provide the ongoing guidance needed for successful relapse prevention.
Final Thoughts
Successful benzodiazepines addiction treatment requires three non-negotiable elements: medical supervision, gradual tapering protocols, and evidence-based therapy. The American Family Physician confirms that abrupt cessation can trigger life-threatening seizures, which makes professional oversight mandatory rather than optional. Recovery timelines extend far beyond initial detox, with full withdrawal symptoms that can persist 10-14 weeks.
Treatment centers report that patients who combine supervised tapering with Cognitive Behavioral Therapy achieve abstinence rates between 25% to 80% (depending on their support systems and housing stability). The most effective programs address both physical dependence and underlying mental health conditions simultaneously. Some patients experience anxiety and sleep disturbances for months after initial withdrawal phases.
We at Amity San Diego provide comprehensive outpatient programs that combine medical oversight with personalized therapy approaches. Our treatment options offer the structured support necessary for long-term recovery while patients maintain their daily responsibilities. Professional benzodiazepines addiction treatment saves lives, as the complexity of withdrawal symptoms and high relapse rates make self-directed recovery dangerous and often unsuccessful.



