Finding the right treatment for co-occurring addiction and mental health disorders requires careful evaluation of integrated treatment programs. These comprehensive approaches address both conditions simultaneously rather than treating them separately.
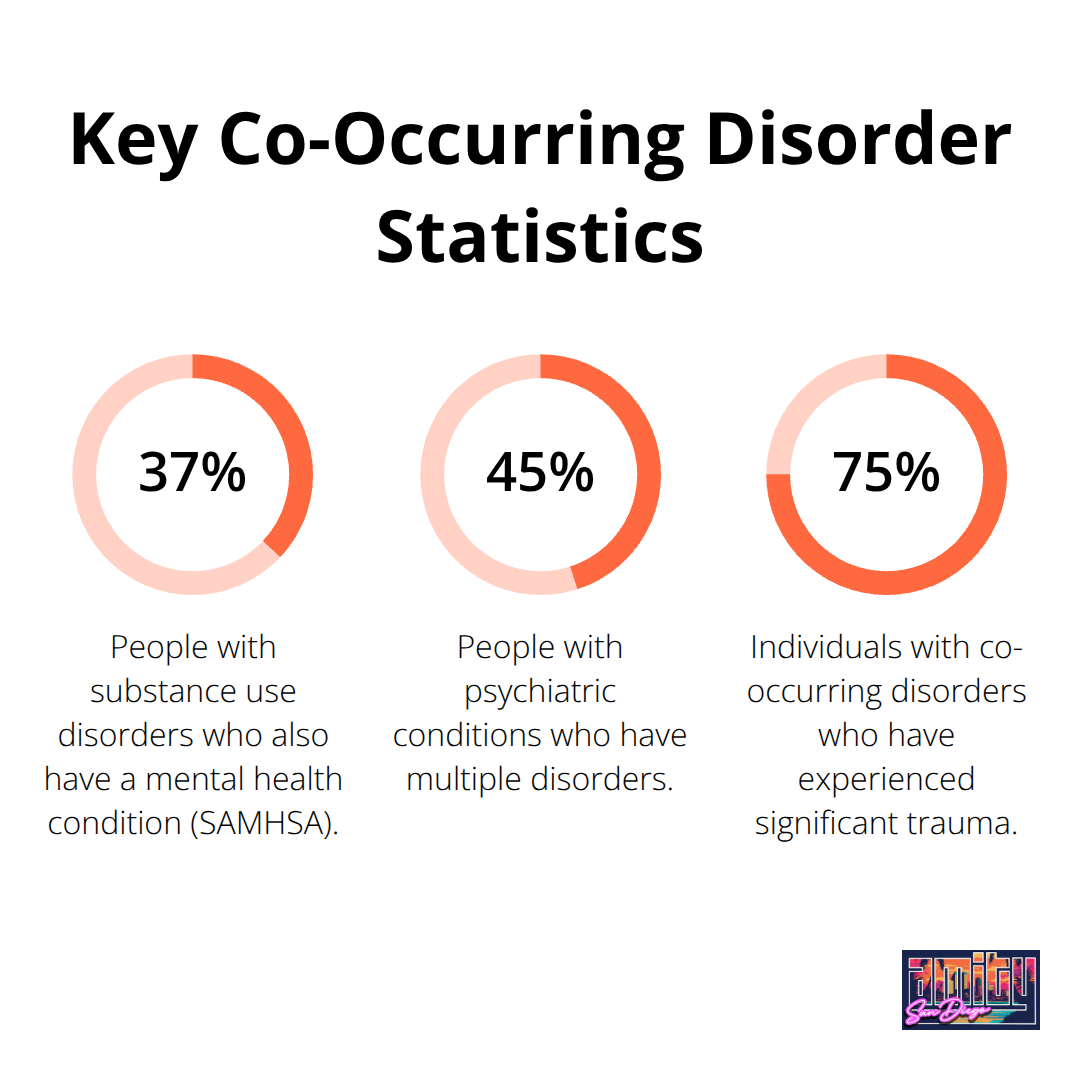
We at Amity San Diego understand that 37% of people with substance use disorders also have mental health conditions, according to SAMHSA data. The wrong program choice can lead to relapse rates exceeding 60% within the first year of treatment.
What Makes Integrated Treatment Different
Integrated treatment programs address addiction and mental health disorders as interconnected conditions rather than separate issues. This approach recognizes that 45% of people with psychiatric conditions have multiple disorders, which makes traditional single-focus treatments inadequate for most clients.
The Science Behind Dual Diagnosis Care
Effective integrated programs combine evidence-based therapies like Cognitive Behavioral Therapy and Dialectical Behavior Therapy with medication management under one clinical team. Research demonstrates that clients who receive integrated care show significantly better outcomes in psychiatric symptomatology than those who receive treatment for addiction and mental health separately.
The key lies in simultaneous treatment timing. Clinicians address both conditions during the same sessions with professionals trained in dual diagnosis approaches. Programs must include psychiatric medication management, individual therapy, group sessions, and family involvement to meet the complex needs of dual diagnosis clients.
Why Single-Focus Treatment Programs Fail
Traditional programs that treat only addiction or only mental health create dangerous gaps in care. Dual diagnosis clients face significant challenges in single-focus programs because underlying psychiatric symptoms trigger substance use when left untreated.
Mental health symptoms like depression, anxiety, or PTSD often drive the initial substance use. When programs address addiction without treating these root causes, relapse becomes inevitable. Conversely, mental health treatment without addressing substance use patterns fails because active addiction prevents therapeutic progress and reduces medication effectiveness.
Key Components That Define Quality Integration
Quality integrated programs share specific characteristics that separate them from standard treatment approaches. Licensed clinical staff must hold dual diagnosis expertise rather than specialization in just one area. The treatment team coordinates care through regular communication and shared treatment plans.
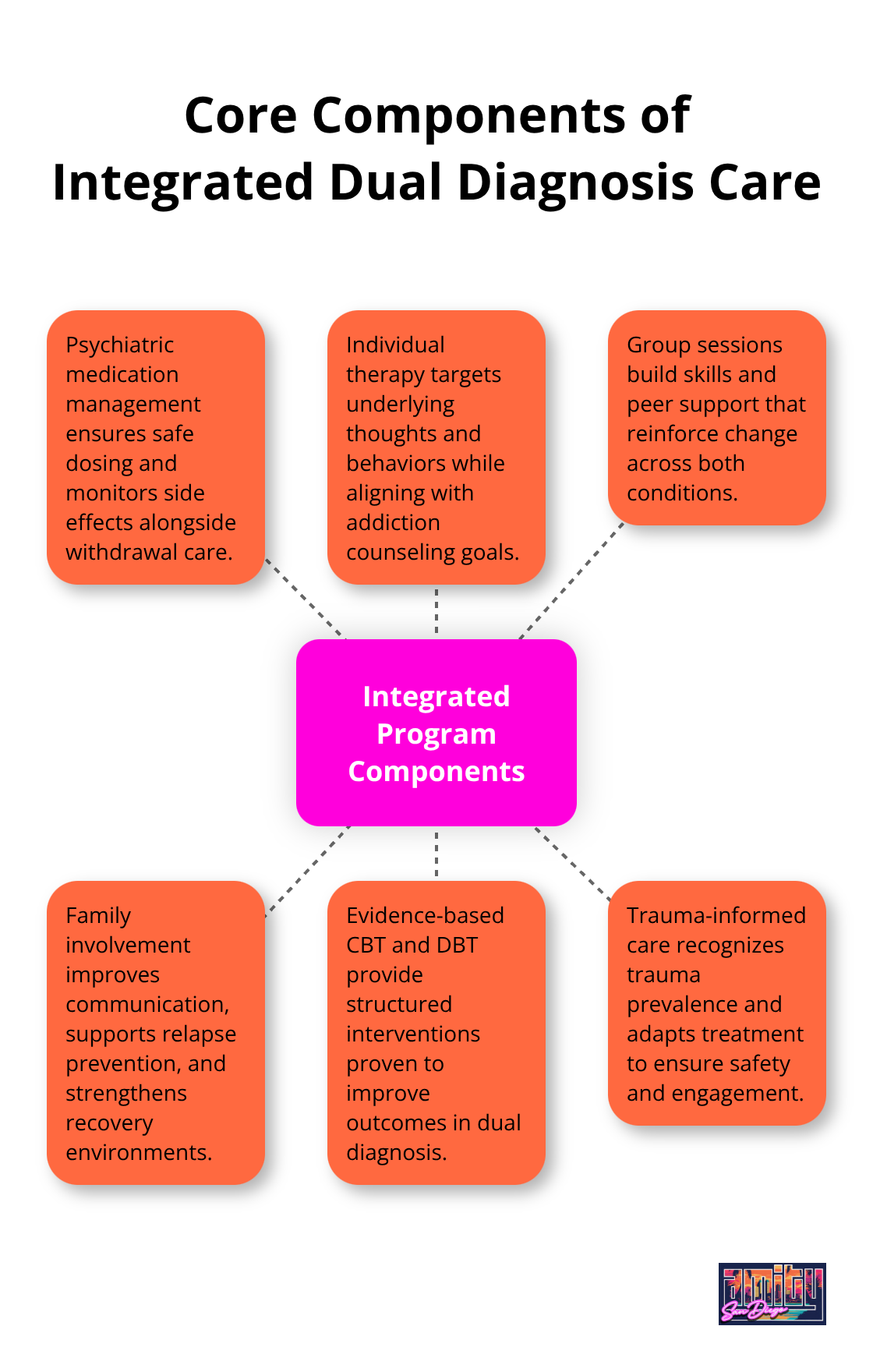
Evidence-based modalities form the foundation of effective programs. These include cognitive behavioral interventions, motivational interviewing techniques, and trauma-informed approaches that address both conditions simultaneously. Medical support remains available throughout treatment to manage withdrawal symptoms and psychiatric medications safely.
When you evaluate potential treatment centers, these foundational elements will help you identify programs that can address your specific needs comprehensively. For comprehensive addiction treatment San Diego options, consider facilities that offer these integrated approaches.
Essential Features of Quality Integrated Programs
Licensed clinical staff with dual diagnosis expertise represent the foundation of effective integrated treatment programs. Social workers increasingly are seeking information about evidence-based practices, making qualified staff selection the most important factor in program evaluation.
Staff Qualifications That Predict Success
Look for programs where clinical directors hold both addiction and mental health credentials, such as Licensed Clinical Social Workers with Certified Addiction Counselor designations. The treatment team should include psychiatrists who specialize in dual diagnosis rather than general practitioners who attempt to manage complex cases.
Research shows that programs with specialized dual diagnosis staff achieve better outcomes. The annual turnover rate was 33.2% for counselors and 23.4% for clinical supervisors, highlighting the importance of staff stability. Verify that nursing staff holds psychiatric nursing certifications, as medical management becomes critical during early treatment phases when psychiatric medications require careful monitoring alongside withdrawal management.
Evidence-Based Treatment Integration
Quality programs implement Cognitive Behavioral Therapy and Dialectical Behavior Therapy as core treatment modalities rather than supplementary options. These therapies must run concurrently with addiction counseling sessions, not as separate mental health services.
Recent studies with experimental or quasi-experimental designs support the effectiveness of integrated dual diagnosis treatments for clients with severe conditions. The clinical team should demonstrate experience in trauma-informed care, as 75% of individuals with co-occurring disorders have experienced significant trauma (according to the National Council for Mental Wellbeing).
Medical Support and Medication Management
Medication-assisted treatment options require on-site medical supervision with psychiatric oversight, not referrals to external providers who lack context about your comprehensive treatment plan. Board-certified physicians must coordinate with psychiatric specialists to manage both withdrawal symptoms and mental health medications simultaneously.
Programs that separate medical care from psychological treatment create dangerous gaps in communication that can lead to medication interactions or inadequate symptom management. The medical team should maintain direct communication with therapists and counselors to adjust treatment protocols based on your progress in both areas.
When you evaluate these staff qualifications and treatment approaches, you’ll need to ask specific questions about how programs coordinate care and verify their claims about integrated services. For comprehensive addiction treatment San Diego options, consider facilities that meet these essential criteria.
How to Evaluate Treatment Centers
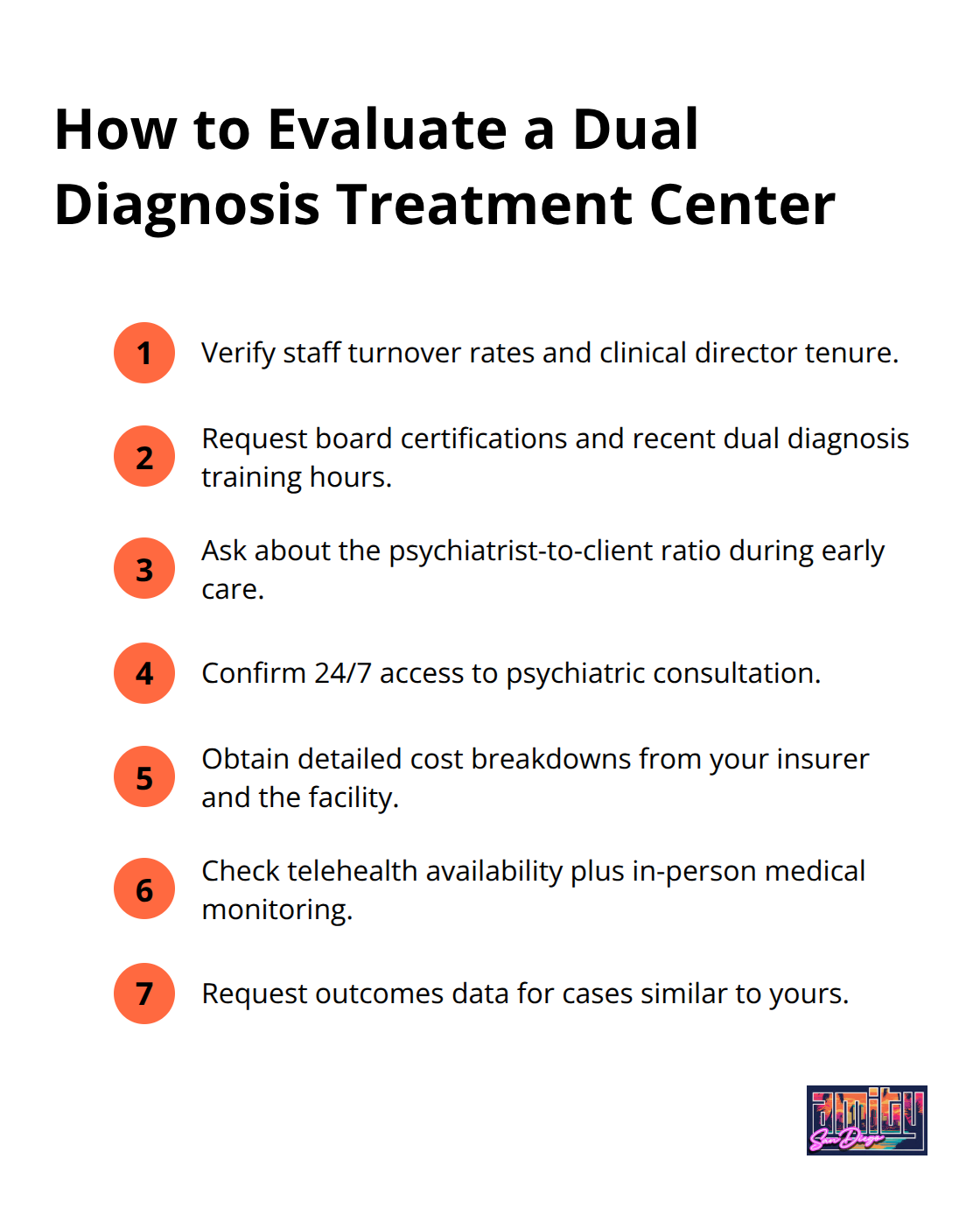
Start with questions about staff turnover rates and average tenure of clinical directors, as facilities with high turnover cannot provide consistent care for dual diagnosis clients. Request specific credentials for psychiatrists and therapists, including board certifications and dual diagnosis training hours completed within the past two years. Ask how many clients with your exact combination of disorders they have treated successfully in the last 12 months, and request outcome data rather than testimonials.
Staff Qualifications and Treatment Approaches
Verify that clinical directors hold active licenses in both addiction counseling and mental health treatment. Ask about the psychiatrist-to-client ratio, as effective dual diagnosis care requires frequent medical consultations during early treatment phases. Request information about how the clinical team coordinates care between addiction counselors and mental health therapists.
Ask about crisis intervention protocols and after-hours medical support availability. Quality alternative drug treatment programs maintain 24/7 access to psychiatric consultation, not just emergency room referrals. Inquire about staff training in trauma-informed care, as most dual diagnosis clients have experienced significant trauma that affects treatment outcomes.
Insurance Coverage and Hidden Costs
Contact your insurance provider directly to verify coverage before trusting facility estimates, as many programs overstate benefits to secure admissions. Request detailed cost breakdowns that include all fees for medical consultations, psychiatric evaluations, and medication management, not just therapy sessions. Mental health and substance use disorder treatment spending continues to grow annually, with integrated programs typically requiring higher investment than single-focus approaches.
Ask about payment plans for portions not covered, as financial stress during treatment increases relapse risk. Verify whether the facility accepts your specific insurance plan or requires out-of-network payments that could create financial barriers to completion.
Location and Schedule Flexibility
Choose facilities within reasonable distance of your home or workplace, as accessibility affects program completion rates. Verify that programs offer evening and weekend sessions if you work traditional hours, since inflexible schedules force many professionals to choose between career stability and recovery.
Ask about telehealth options for individual sessions during work travel or emergencies, but avoid programs that rely primarily on virtual care for dual diagnosis treatment. In-person medical monitoring remains essential for medication management and crisis intervention during early recovery phases. For comprehensive addiction treatment San Diego residents can access specialized dual diagnosis programs that combine both approaches effectively.
Final Thoughts
Effective integrated treatment programs require three fundamental elements: qualified dual diagnosis staff, coordinated medical care, and accessible treatment schedules. Programs with licensed specialists who treat addiction and mental health simultaneously produce better outcomes than facilities that address these conditions separately. Your choice should prioritize centers where psychiatrists collaborate directly with addiction counselors rather than operate through disconnected departments.
Quality facilities maintain low staff-to-client ratios and provide trauma-informed care as standard practice. Verify insurance coverage independently and ask specific questions about staff turnover rates and crisis intervention protocols (these factors directly impact treatment continuity). The right program offers both Partial Hospitalization and Intensive Outpatient options to match your recovery phase.
We at Amity San Diego provide evidence-based dual diagnosis treatment through our PHP and IOP programs. Our clinical team coordinates comprehensive care for clients with co-occurring disorders. Contact us today for a confidential assessment to begin your recovery with addiction treatment San Diego specialists.



