Finding the right dual diagnosis treatment programs can feel overwhelming when you’re dealing with both mental health and substance use challenges simultaneously.
We at Amity San Diego understand that effective treatment requires specialized care that addresses both conditions together, not separately. The right program makes all the difference in achieving lasting recovery and mental wellness.
What Makes Dual Diagnosis Treatment Different
Dual diagnosis treatment addresses the complex reality that approximately 21.2 million adults face both mental illness and substance use disorders simultaneously, according to the Substance Abuse and Mental Health Services Administration. This represents two interconnected problems that feed off each other in ways that make traditional single-focus treatment approaches fail consistently. Depression drives someone to drink more heavily, while alcohol abuse worsens depressive symptoms, which creates a destructive cycle that requires specialized intervention.
The Most Common Dual Diagnosis Combinations
The National Institute on Drug Abuse reports that people with substance use disorders often have co-occurring mental health conditions. Depression paired with alcohol use disorder represents the most frequent combination that treatment facilities see across the country. Anxiety disorders commonly occur alongside benzodiazepine abuse, while PTSD frequently drives opioid dependence as people attempt to numb traumatic memories. Bipolar disorder creates particularly challenging scenarios when combined with stimulant abuse (as manic episodes can trigger dangerous drug binges that spiral out of control).
Why Integrated Care Beats Sequential Treatment
Research from Norwegian Community Mental Health Centres shows that integrated treatment significantly improves patient motivation compared to separate condition treatment. When you address mental health first and substance abuse later (or vice versa), you essentially treat half the problem while the other half sabotages your progress. Integrated approaches use the same treatment team to simultaneously tackle both conditions, which prevents the communication gaps and conflicting advice that derail recovery efforts.
The Science Behind Integrated Treatment Success
Studies demonstrate that people who receive integrated care experience fewer hospitalizations, better medication compliance, and dramatically lower relapse rates than those who bounce between separate mental health and addiction specialists. The Alcohol Use Disorder Identification Test and Drug Use Disorder Identification Test show statistically significant reductions in substance use over 12 months when patients receive coordinated care. This evidence points to a clear advantage: comprehensive programs that treat the whole person rather than isolated symptoms produce measurably better outcomes.
These proven benefits make program selection critical for anyone seeking addiction treatment San Diego.
Key Features of Effective Dual Diagnosis Programs
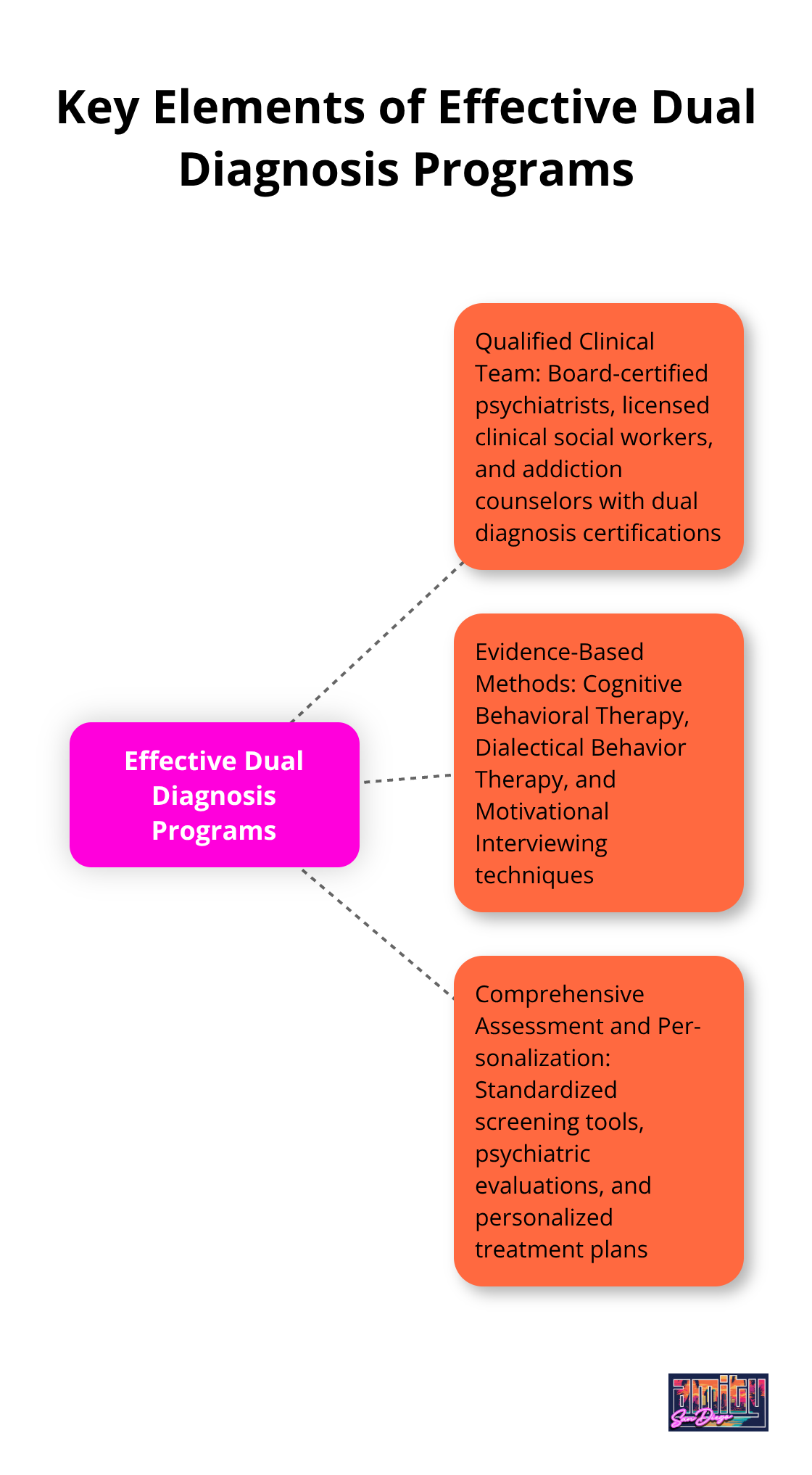
Effective dual diagnosis programs stand apart through three non-negotiable elements that determine treatment success. The clinical team must include board-certified psychiatrists, licensed clinical social workers, and addiction counselors who hold specific dual diagnosis certifications. The purpose of credentialing is to standardize the quality of addiction prevention, intervention, treatment and continuing care services. Generic mental health or addiction training alone creates dangerous knowledge gaps that lead to misdiagnosis and treatment failures.
Staff Qualifications That Matter
Staff should complete at least 40 hours of continuing education annually in integrated treatment approaches. The program should maintain a maximum 8-to-1 client-to-therapist ratio to provide adequate individual attention. Look for facilities where psychiatrists conduct evaluations within 48 hours of admission rather than weeks later. Licensed clinical social workers should have specialized training in both addiction counseling and mental health treatment (not just one area of expertise).
Evidence-Based Methods That Actually Work
Cognitive Behavioral Therapy and Dialectical Behavior Therapy form the backbone of successful dual diagnosis treatment. CBT for substance use disorders has demonstrated efficacy as both a monotherapy and as part of combination treatment strategies. Programs should offer Motivational Interviewing techniques and trauma-focused therapies like EMDR for clients with PTSD-related substance abuse.
Medication-Assisted Treatment Integration
Medication-Assisted Treatment integration becomes essential when opioid use disorders combine with depression or anxiety. The program should provide detailed documentation of which specific therapeutic modalities they use and how these methods address both conditions simultaneously rather than alternating focus between mental health and addiction. Staff must understand medication interactions between psychiatric drugs and substances of abuse.
Assessment and Personalization Requirements
Comprehensive intake assessments must include standardized screening tools like the Alcohol Use Disorder Identification Test and psychiatric evaluations conducted by licensed psychiatrists. The AUDIT is a 10-item screening tool developed by the World Health Organization to assess alcohol use disorders. Programs that skip psychiatric evaluation or rely solely on self-reporting create treatment plans based on incomplete information. The assessment process should identify specific medication interactions, trauma history, and previous treatment failures to avoid repeating ineffective approaches.
Treatment plans require weekly updates based on progress metrics, and programs should provide written documentation of how they modify interventions when clients show resistance or poor response to initial treatment strategies. These assessment standards help you evaluate whether a program can deliver the comprehensive care you need. For those seeking specialized addiction treatment San Diego offers quality dual diagnosis programs.
How Do You Choose the Right Dual Diagnosis Program?
Essential Questions That Reveal Program Quality
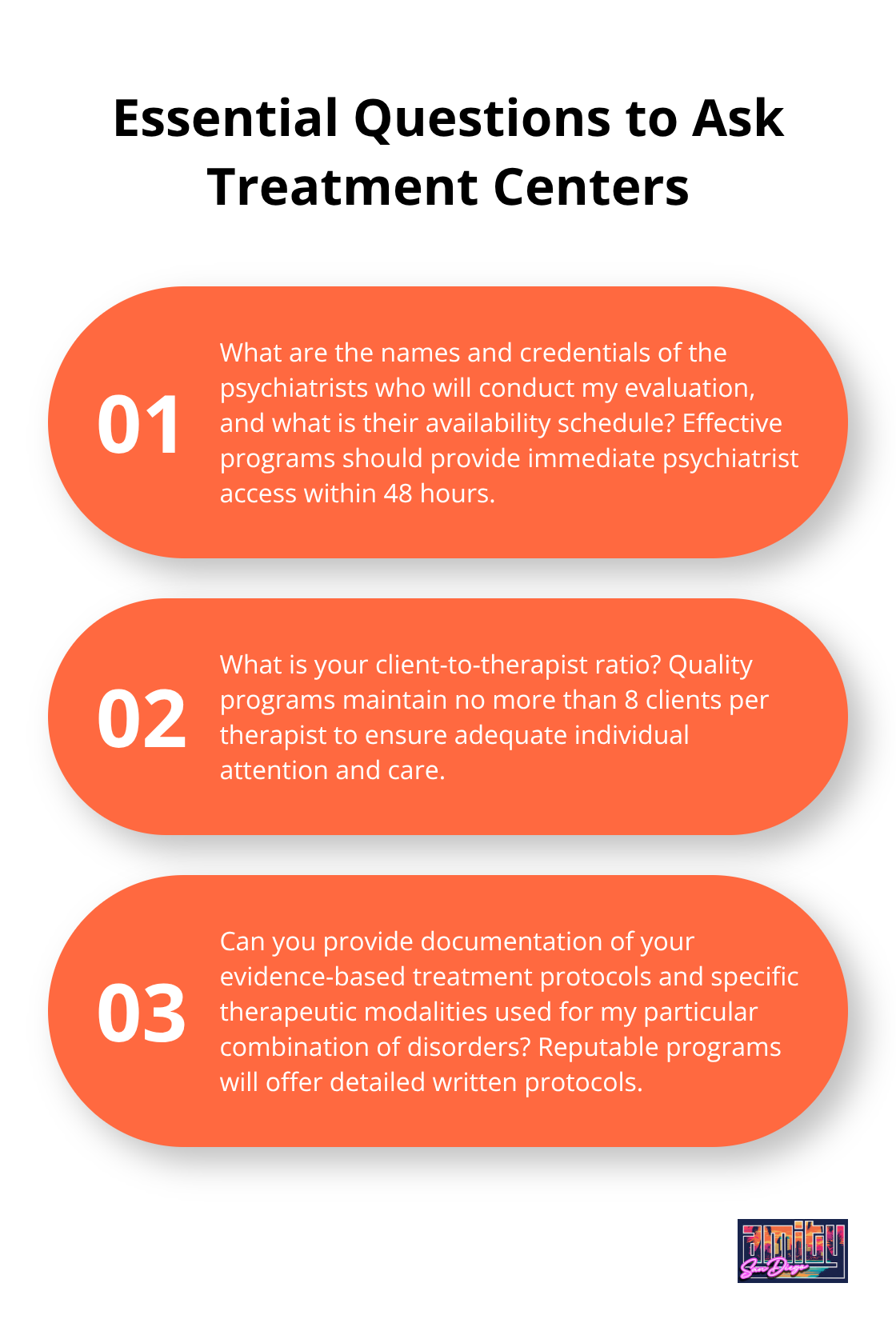
Ask treatment centers specific questions that expose their actual capabilities rather than marketing claims. Request the names and credentials of psychiatrists who will conduct your evaluation, and demand to know their availability schedule. Programs that cannot provide immediate psychiatrist access within 48 hours lack the medical oversight necessary for dual diagnosis treatment. Ask for their client-to-therapist ratio numbers, as effective programs maintain no more than 8 clients per therapist. Request documentation of their evidence-based treatment protocols and ask which specific therapeutic modalities they use for your particular combination of disorders. Quality dual diagnosis programs will provide detailed written protocols rather than vague descriptions of their approach.
Insurance Coverage Reality Check
Insurance coverage for dual diagnosis treatment varies dramatically between mental health and substance abuse benefits, with mental health treatment typically receiving better coverage. According to SAMHSA’s 2022 National Survey on Drug Use and Health, approximately 21.5 million adults in the United States have a co-occurring disorder. Contact your insurance company directly to verify both your mental health and substance abuse benefits, as treatment centers often provide incomplete coverage information. Request written pre-authorization for the specific dual diagnosis program you consider, not just general addiction treatment approval. The current cost ranges between $4,008 and $15,524 for adult residential treatment, while therapeutic community treatment costs between $14,818 and $32,361. Programs should provide transparent pricing and payment plans rather than refuse to discuss costs until after admission.
Location and Care Level Decisions
Choose programs within 50 miles of your support system, as geographical proximity to family and friends significantly impacts recovery success rates. Intensive outpatient programs can be effective treatment options, with studies showing substantial reductions in alcohol and drug use between baseline and follow-up. Residential treatment becomes necessary when previous outpatient attempts have failed or when severe psychiatric symptoms require 24-hour monitoring (particularly for individuals with active suicidal ideation). Programs should offer multiple levels of care including partial hospitalization, intensive outpatient, and standard outpatient options to provide step-down care as you progress. Avoid programs that only offer one level of care, as your needs will change throughout recovery and you should not have to switch facilities to access different intensity levels.
Staff Credentials and Treatment Approach Verification
Verify that clinical staff hold current licenses in both addiction counseling and mental health treatment. Ask for specific examples of how they modify treatment plans when clients show resistance or poor response to initial interventions. Request information about their continuing education requirements (quality programs require at least 40 hours annually in integrated treatment approaches). Programs should demonstrate how they coordinate care between psychiatrists, therapists, and medical staff rather than operate these services independently. Quality facilities will provide written documentation of their integrated treatment model and explain how they prevent the communication gaps that sabotage recovery efforts. For those seeking comprehensive care, consider addiction treatment San Diego options that provide integrated dual diagnosis services.
Final Thoughts
Specialized dual diagnosis treatment programs represent the most important decision you can make for lasting recovery. The statistics speak clearly: people with co-occurring disorders who receive integrated care experience significantly better outcomes than those who attempt to address mental health and substance abuse separately. The 21.2 million Americans who face both conditions simultaneously need comprehensive treatment that addresses the root causes of both disorders.
The first step requires courage, but you don’t have to navigate this process alone. Contact your insurance company to verify coverage for dual diagnosis treatment, then research programs that meet the quality standards we’ve outlined. Look for facilities with board-certified psychiatrists, licensed clinical staff with specialized training, and evidence-based treatment protocols (these elements determine treatment success rates).
We at Amity San Diego provide integrated outpatient care that combines medical interventions with personalized, trauma-informed treatment. Our multidisciplinary team understands the complex relationship between mental health and substance use disorders. Recovery becomes possible when you receive the specialized care that addresses your complete health picture rather than treats symptoms in isolation through addiction treatment San Diego programs.



