Medi-Cal addiction treatment coverage can help you access the care you need without overwhelming financial burden. Many people don’t realize the full scope of services available through this program.
We at Amity San Diego see firsthand how proper coverage knowledge transforms recovery outcomes. This guide walks you through finding and accessing Medi-Cal benefits for addiction treatment.
What Does Medi-Cal Cover for Addiction Treatment
Medi-Cal provides comprehensive addiction treatment coverage that includes detoxification, inpatient residential care, outpatient programs, and medication-assisted treatment. The program covers both medical detox services and residential treatment for up to 30 days when medically necessary, with prior authorization required for residential stays. Outpatient services include individual and group counseling, intensive outpatient programs that offer 9-19 hours of weekly treatment for adults, and standard outpatient care with up to 9 hours per week. According to the California Department of Health Care Services, over 12 million Californians currently hold Medi-Cal coverage, which makes these services accessible to a substantial population that faces substance use disorders.
Inpatient vs Outpatient Coverage Differences
Residential inpatient treatment requires prior authorization and medical necessity documentation, while outpatient services receive automatic coverage for eligible members. The Drug Medi-Cal Organized Delivery System covers 96% of Medi-Cal recipients in California and provides 24/7 access to services through member access lines.

Inpatient programs offer 24-hour non-medical rehabilitation in residential settings (typically lasting 30 days based on statewide averages). Outpatient options include narcotic treatment programs available seven days per week for individuals aged 12 and older, plus peer mentorship services that connect patients with recovery coaches who have lived experience.
Mental Health and Dual Diagnosis Support
Medi-Cal recognizes that California had 10,898 all drug-related overdose deaths in 2021, which highlights the need for integrated treatment approaches. The program covers co-occurring mental health disorders alongside addiction treatment and provides access to licensed clinicians who specialize in dual diagnosis care. Behavioral Health Integration services combine treatment for both conditions simultaneously and follow evidence-based practices that significantly improve recovery outcomes.
Medication-Assisted Treatment Options
Medi-Cal covers FDA-approved medications like methadone, buprenorphine, and naltrexone for opioid use disorder treatment. These medications help reduce withdrawal symptoms and cravings (which are essential components of successful recovery). Narcotic Treatment Programs operate seven days per week and integrate counseling with medication management to provide comprehensive care for individuals with opioid addiction.
Now that you understand what Medi-Cal covers, the next step involves verifying your eligibility and locating approved providers in your area. For those seeking comprehensive addiction treatment San Diego options, understanding these coverage details can help guide your treatment decisions.
How to Check Your Medi-Cal Eligibility and Benefits
Call the Medi-Cal Member Services line at 1-800-541-5555 to confirm your active enrollment status and coverage details. The California Department of Health Care Services also provides online verification through their BenefitsCal website, where you can log in with your case number and review your current benefits package. Your Medi-Cal identification card displays your member ID number (which you’ll need when you contact treatment providers to verify coverage for addiction services).
Steps to Verify Your Current Medi-Cal Status
Access your account through the BenefitsCal portal or call the member services hotline to check your enrollment dates and benefit levels. Verify that your coverage remains active and note any restrictions or limitations that might affect addiction treatment services. The system will show you which services require prior authorization and which receive automatic approval for eligible members.
How to Find Covered Treatment Providers in Your Area
The SAMHSA Treatment Locator at findtreatment.gov allows you to search specifically for Medi-Cal-certified addiction treatment facilities within your zip code. California’s Drug Medi-Cal Organized Delivery System maintains provider directories that list facilities that accept Medi-Cal for substance use disorder treatment, complete with contact information and services offered. Contact potential providers directly and ask three specific questions: Do you accept Medi-Cal for addiction treatment, what is your current wait time for new patients, and do you require prior authorization for the level of care you need. While Medi-Cal covers a broad range of services, not all treatment centers accept it, so always verify with the treatment provider before starting a program.
Understanding Prior Authorization Requirements
Residential treatment programs require prior authorization based on medical necessity, while outpatient services receive automatic approval for eligible Medi-Cal members. Your treatment provider typically handles the prior authorization process, but you should understand that approval depends on whether you meet American Society of Addiction Medicine criteria for placement decisions. Intensive outpatient programs that offer 9-19 hours weekly for adults generally receive faster approval than residential stays.
What to Do If Coverage Gets Denied
California’s Department of Health Care Services allows appeals through a formal process that can overturn coverage decisions when medical necessity is properly documented. Submit your appeal within 60 days of the denial notice and include additional medical documentation that supports your need for treatment. The Orange County Behavioral Health Services offers 24/7 access through their Member Access Line at 800-723-8641, which can connect you to treatment services and help navigate coverage issues.
Once you verify your coverage and locate approved providers, the next step involves researching specific treatment centers to find quality care that meets your recovery needs. For those seeking comprehensive addiction treatment San Diego options, professional guidance can help navigate both coverage requirements and treatment selection.
Finding Quality Medi-Cal Approved Treatment Centers
Start your search with the California Department of Health Care Services provider directory and cross-reference facilities with state boards to verify accreditation status. The Joint Commission maintains a database of accredited facilities, and you should only consider centers that hold both state certification and national accreditation. Contact each facility directly and ask these specific questions: What is your current wait time for new Medi-Cal patients, do you provide transportation assistance, what happens if I need a higher level of care during treatment, and can you provide references from recent Medi-Cal patients who completed your program. According to the Substance Abuse and Mental Health Services Administration, only 11% of individuals with substance use disorders received treatment in 2019 (which means quality providers often have wait lists).
Research Accredited Facilities That Accept Medi-Cal
Verify that treatment centers hold current state certification through the California Department of Health Care Services and maintain national accreditation from recognized organizations. Check the facility’s license status on the California Department of Public Health website and confirm they accept Medi-Cal for the specific level of care you need. Quality centers will provide their certification numbers without hesitation and explain their treatment philosophy during initial consultations.
Warning Signs That Indicate Poor Treatment Quality
Avoid facilities that guarantee recovery outcomes, demand large upfront payments despite Medi-Cal coverage, or pressure you to sign contracts before you tour their facility. Red flags include unlicensed staff who provide clinical services, facilities that refuse to provide verification numbers, centers that discourage family involvement without medical justification, and programs that promise luxury amenities while accepting Medi-Cal without explanation of how they fund these extras.
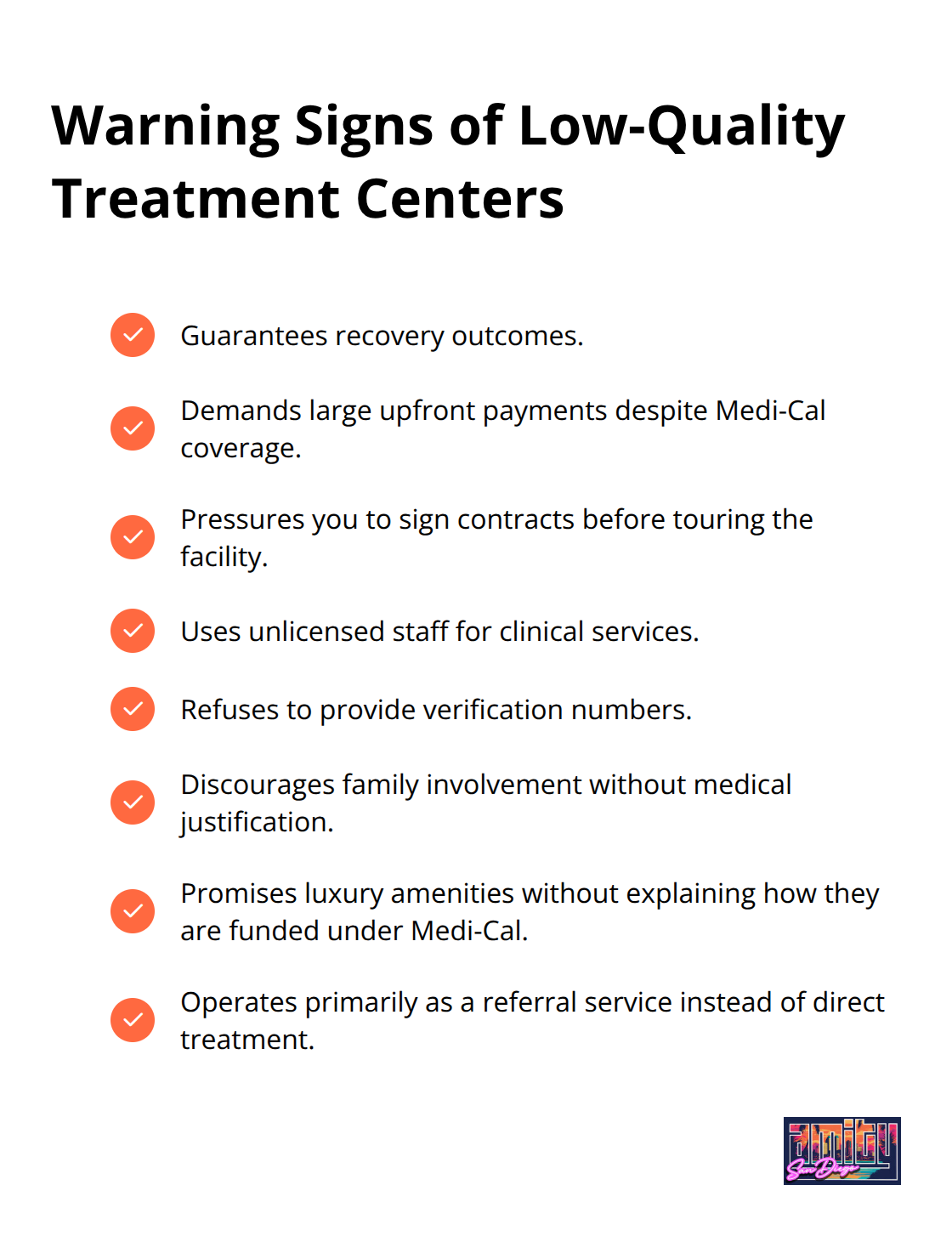
The California Department of Health Care Services reports that legitimate providers will always verify their certification status and explain their treatment approach during initial consultations. Facilities that operate primarily as referral services rather than direct treatment should raise immediate concerns about their commitment to patient care.
Essential Questions for Treatment Provider Interviews
Ask about staff-to-patient ratios, average length of stay for patients with similar conditions, and specific evidence-based therapies they use beyond basic counseling. Request information about their discharge plans, alumni support programs, and how they handle medical emergencies or psychiatric crises. The ASAM Criteria should guide their placement decisions, and quality providers will explain how they assess your treatment needs. Contact treatment providers who offer transparent outcome data and evidence-based approaches that align with your recovery goals, which represents the type of specific information legitimate providers should readily share about their treatment approach and expected outcomes.
Final Thoughts
You can access Medi-Cal addiction treatment through three steps: verify your eligibility through BenefitsCal or call 1-800-541-5555, locate certified providers with the SAMHSA Treatment Locator, and research facilities that hold proper accreditation. The Drug Medi-Cal Organized Delivery System covers 96% of recipients and provides 24/7 access to services.

This makes treatment more accessible than many people realize.
County behavioral health departments and community-based organizations offer additional financial assistance beyond Medi-Cal coverage. The California Health Care Foundation advocates for improved access and provides resources for individuals who need help with the application process. These organizations help people navigate coverage complexities that often prevent them from starting treatment.
Your recovery starts when you contact treatment providers to verify coverage and ask about wait times for new patients. We at Amity San Diego understand that finding quality care can feel overwhelming (which is why we offer free confidential assessments to help you understand your options). Contact us today to learn more about our addiction treatment San Diego programs and verify your Medi-Cal addiction treatment coverage.



