Ibogaine treatment for addiction represents one of the most controversial yet promising approaches in recovery medicine. This plant-derived psychoactive compound has shown remarkable results in breaking addiction cycles, particularly for opioid dependence.
At Amity San Diego, we understand the complexity of addiction recovery and the need for innovative treatment options. The growing interest in ibogaine stems from its unique ability to reset brain chemistry and reduce withdrawal symptoms in ways traditional methods cannot match.
What Is Ibogaine Treatment
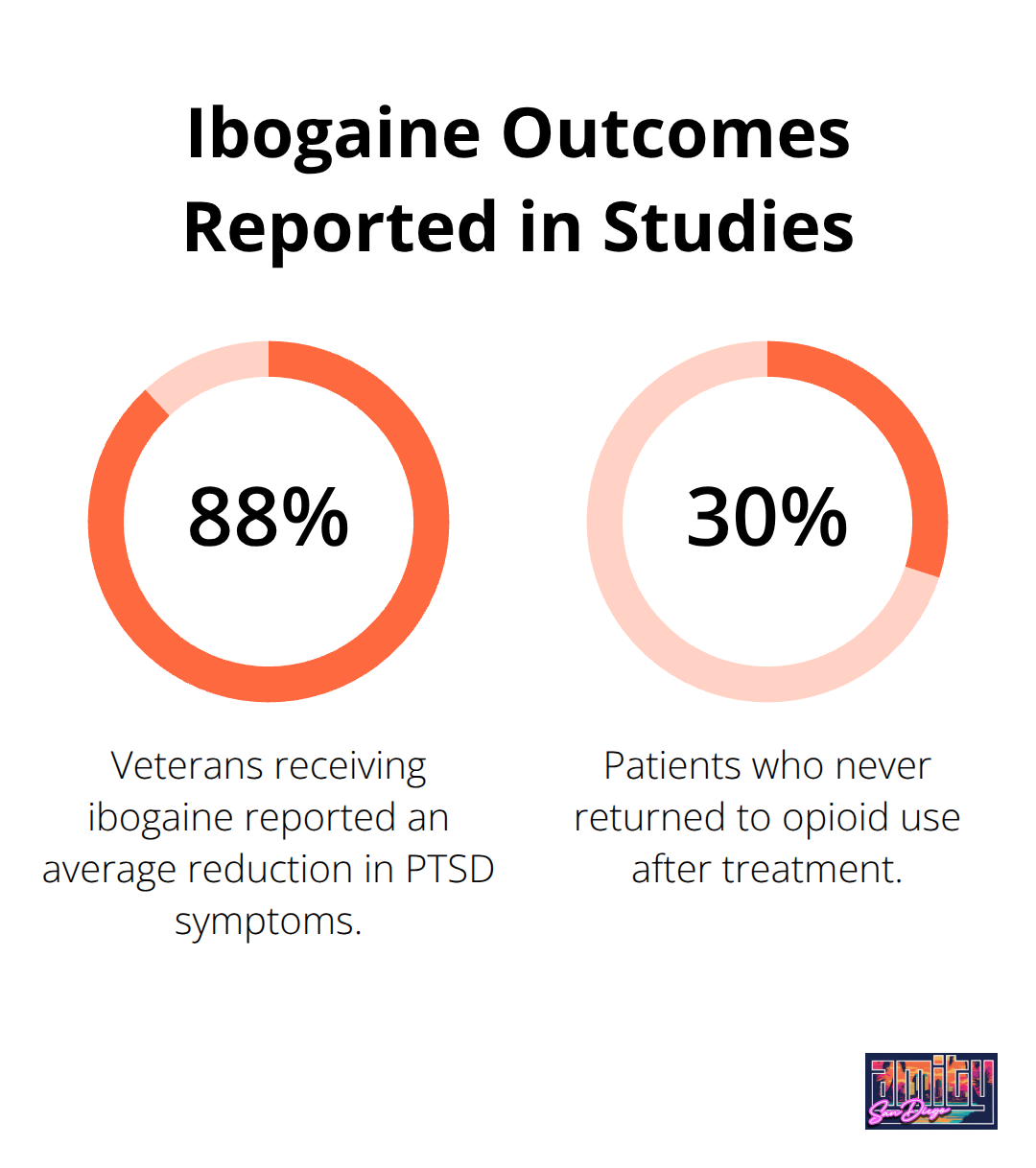
Ibogaine is a naturally occurring psychoactive alkaloid that scientists extract from the root bark of the Tabernanthe iboga plant, native to West and Central Africa. The Bwiti people have used this compound in spiritual ceremonies for centuries, but modern medicine has transformed it into a potential addiction treatment. Stanford Medicine researchers found that veterans who received ibogaine experienced an average 88% reduction in PTSD symptoms, while studies show 30% of patients never returned to opioid use after treatment.
The Science Behind Ibogaine’s Brain Effects
Ibogaine targets multiple neurotransmitter systems simultaneously, particularly the serotonin transporter and dopamine pathways that addiction hijacks. Research from UCSF shows ibogaine affects brain wave patterns and increases theta rhythms linked to improved executive function. The compound essentially resets neural pathways that substance abuse damages, with participants who show measurable changes in brain activity complexity. Studies indicate that 80% of patients experience reduced withdrawal symptoms immediately after treatment, with effects that last at least one month.
Why Traditional Treatments Fall Short
Traditional addiction treatments like methadone maintenance and behavioral therapy show success rates of only 20-30% for long-term recovery. Ibogaine offers a radically different approach-rather than manage addiction symptoms indefinitely, it appears to interrupt the addiction cycle entirely. While conventional treatments require daily medication or weekly therapy sessions for years, ibogaine can produce effects that last from a single treatment session. This power comes with significant risks that require comprehensive medical supervision.
The Treatment Process Overview
Medical professionals administer ibogaine in controlled clinical settings where they monitor patients for 24-48 hours. The average dose ranges between 15-20 mg/kg (depending on individual factors), and patients receive extensive cardiac supervision throughout the experience. Most participants report visual phenomena or hallucinations during the session, with 88% experiencing these altered states of consciousness. The treatment process demands thorough medical screening beforehand to identify suitable candidates and minimize potential complications.
The Ibogaine Treatment Process
Medical professionals divide ibogaine treatment into three distinct phases that determine patient outcomes. Pre-treatment screening eliminates candidates due to cardiovascular risks, psychiatric contraindications, or medication interactions that could prove fatal. Medical teams conduct comprehensive cardiac evaluations (including EKGs, echocardiograms, and stress tests), while psychiatric assessments identify conditions like bipolar disorder or schizophrenia that disqualify candidates. Laboratory work screens for liver function, kidney health, and drug interactions, with particular attention to medications like SSRIs that patients must discontinue weeks before treatment.
Pre-Treatment Medical Assessment
Thorough medical evaluation forms the foundation of safe ibogaine treatment. Physicians require complete cardiovascular workups since ibogaine affects heart rhythm and can cause dangerous arrhythmias in susceptible patients. Blood tests reveal liver enzyme levels, kidney function markers, and electrolyte imbalances that could complicate treatment. Mental health professionals screen for psychiatric conditions that ibogaine might worsen, particularly psychotic disorders or severe personality disorders that contraindicate psychedelic therapy.
The Active Treatment Session
The actual ibogaine session spans 12-36 hours of active effects, with patients receiving doses calculated at less than 1 mg/kg for safe treatment. Medical staff monitor heart rhythm continuously while checking blood pressure and oxygen levels hourly. Patients experience intense visual phenomena and introspective states that 88% describe as transformative, though the physical experience includes nausea, light sensitivity, and temporary coordination difficulties. Professional facilities provide magnesium supplementation to reduce cardiac risks and maintain IV access throughout the session for emergency interventions.
Post-Treatment Medical Monitoring
The immediate 72-hour period after ibogaine requires intensive medical observation. Patients may experience lingering effects including fatigue, mood fluctuations, and continued sensitivity to stimuli. Medical teams monitor for delayed cardiac complications and assess neurological function as the compound clears from the system. Blood pressure stabilization and return of normal coordination mark successful completion of the acute treatment phase.
Integration and Aftercare Planning
The 30-day period following ibogaine treatment determines long-term success rates. Studies show patients who engage in structured aftercare programs maintain abstinence rates with 11% eventually achieving complete abstinence and 47% decreasing use from previous levels.
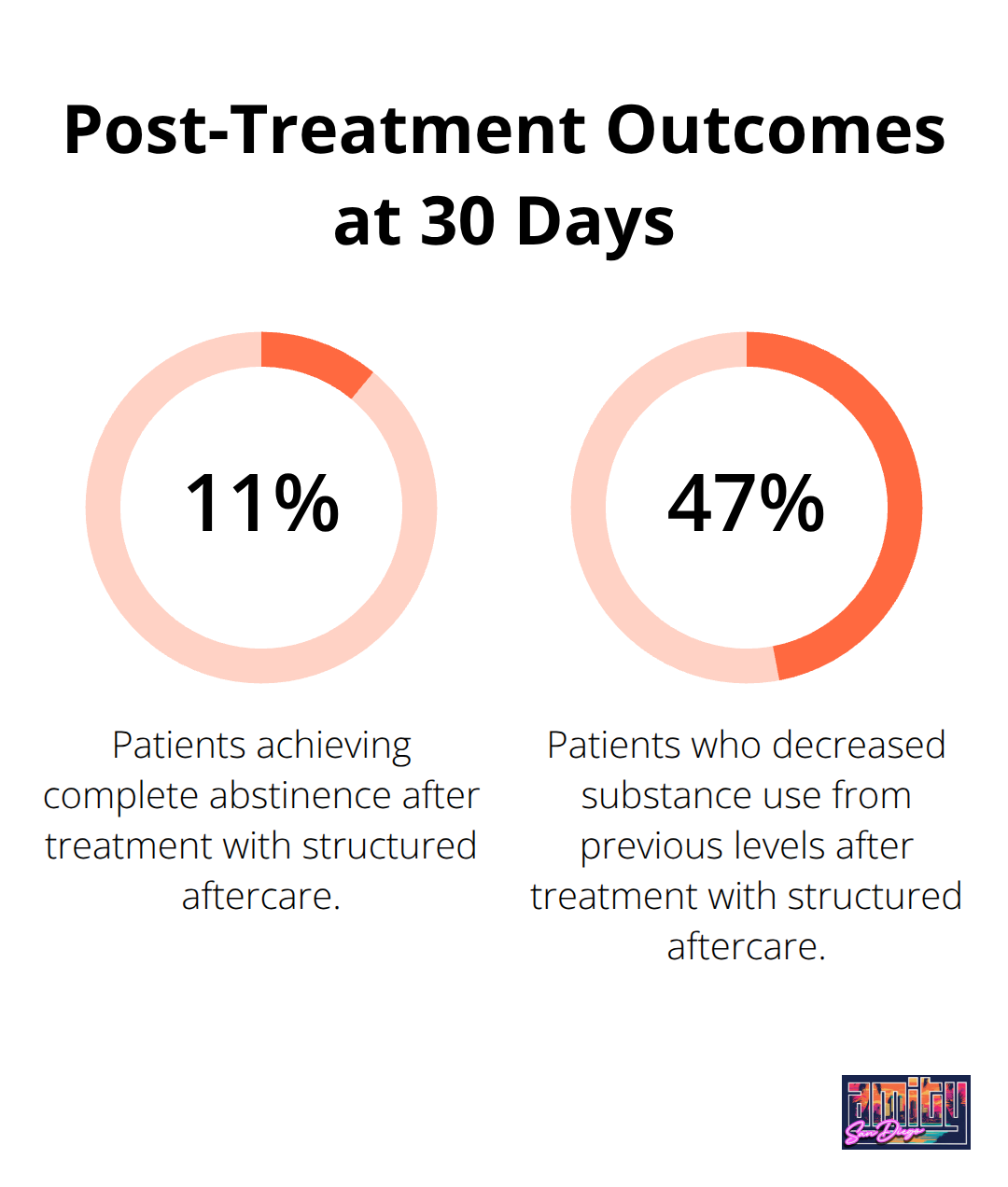
Integration therapy helps process psychological insights from the experience while medical monitoring continues for several weeks to address any persistent effects. However, even the most intensive ibogaine treatment faces significant limitations without comprehensive addiction treatment San Diego programs that address the complex medical and psychological risks inherent in this controversial approach.
Risks and Considerations of Ibogaine Treatment
Cardiac Complications That Can Kill
Ibogaine poses severe cardiac risks that have resulted in 19 documented deaths worldwide from 1990 to 2008. The compound affects heart rhythm by blocking potassium channels, which leads to QT interval prolongation and potentially fatal arrhythmias. Patients with existing cardiovascular conditions face exponentially higher risks, with heart failure being the primary cause of ibogaine-related fatalities.
Medical facilities require comprehensive cardiac screening (including EKGs, echocardiograms, and stress tests) before treatment approval. Magnesium supplementation during treatment reduces cardiac complications, but deaths still occur even in supervised medical settings with continuous monitoring. The cardiac risks make ibogaine one of the most dangerous addiction treatments available today.
Legal Barriers Block Access to Safe Treatment
Ibogaine remains a Schedule I controlled substance in the United States, which makes possession and distribution illegal with severe criminal penalties. This legal status forces Americans to seek treatment in Mexico, Canada, or other countries where regulation varies dramatically. Many individuals have traveled abroad for ibogaine treatment, often to facilities with questionable medical oversight and safety protocols.
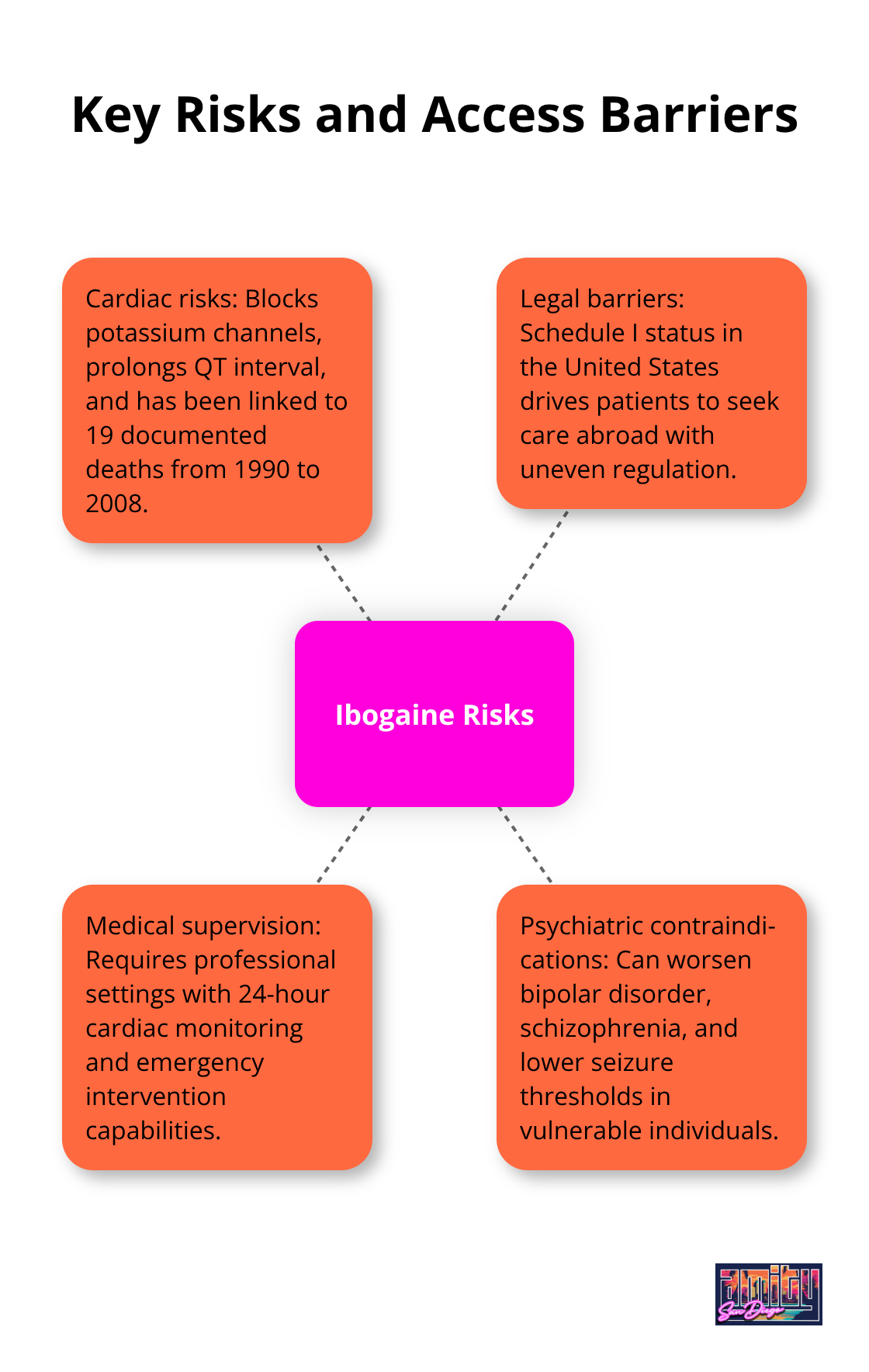
The lack of FDA oversight means no standardized dosing, preparation methods, or safety protocols exist. Quality control issues plague the international ibogaine market, with contaminated or mislabeled products that create additional dangers for patients who seek treatment.
Medical Supervision Prevents Deaths
Professional medical supervision with 24-hour cardiac monitoring represents the only acceptable approach to ibogaine treatment. Facilities must maintain emergency cardiac intervention capabilities (including defibrillators, advanced life support equipment, and immediate access to intensive care units). Qualified medical teams require extensive experience with psychedelic medicine and cardiac emergency management.
Patients need continuous IV access throughout treatment for emergency medication administration if complications arise. The absence of proper medical supervision transforms ibogaine from a potentially therapeutic compound into a life-threatening gamble that has killed dozens of people who sought addiction treatment San Diego.
Psychiatric Contraindications Create Additional Risks
Ibogaine can trigger severe psychiatric episodes in vulnerable individuals, particularly those with bipolar disorder, schizophrenia, or other psychotic conditions. The compound’s intense psychological effects can worsen existing mental health conditions or unmask latent psychiatric disorders. Patients with a history of seizures face increased risks, as ibogaine can lower seizure thresholds and trigger dangerous neurological events.
Final Thoughts
Ibogaine treatment addiction recovery presents both extraordinary promise and serious dangers that demand careful consideration. Research shows 88% reduction in PTSD symptoms and 30% of patients never return to opioid use, yet 19 documented deaths highlight the compound’s lethal potential. The cardiac risks, legal barriers, and psychiatric contraindications make ibogaine one of the most controversial approaches in addiction medicine.
The legal status as a Schedule I substance forces Americans to seek treatment abroad, often in facilities with questionable safety protocols. Even with proper medical supervision, ibogaine can trigger fatal arrhythmias or severe psychiatric episodes in vulnerable individuals. The absence of FDA oversight means no standardized protocols exist for safe administration.
We at Amity San Diego believe recovery requires comprehensive, evidence-based approaches that prioritize patient safety above all else. Our team provides proven therapies in a medically supervised environment (including CBT, DBT, and EMDR through our programs). While ibogaine may offer breakthrough potential for some patients, the risks currently outweigh benefits for most individuals who need addiction treatment San Diego.



